First-In-The-World Trilogy of Radiation Oncology Treatments Boosts Effectiveness for Treating Certain Cancers
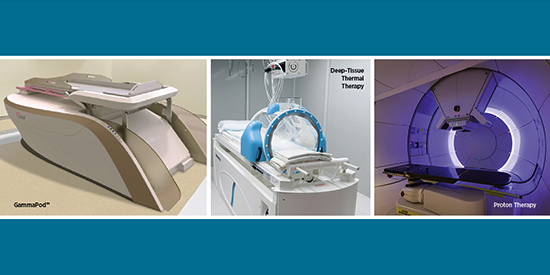
The University of Maryland Medical Center is the only center in the world to offer deep-tissue thermal therapy (also known as hyperthermia), proton therapy, and GammaPod™. Our University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC) patients access unparalleled oncology treatments.
University-based medicine develops innovative cures and treatments not found anywhere else and multi-disciplinary care teams staffed with internationally recognized specialists.
GammaPod
Pioneered for Early-Stage Breast Cancer
Choosing treatment at UMGCCC ensures patients receive the latest options, including treatments invented here such as GammaPod. This new form of partial breast irradiation is proven to be safe and feasible. A variety of clinical trials are available with the potential to improve patient and cosmetic outcomes and improve convenience of care for early-stage breast cancer patients.
GammaPod delivers less radiation to the heart and lungs. Studies have demonstrated that the GammaPod provides a more rapid dose falloff from the targeted area. The rapid falloff was even greater with GammaPod than with intracavitary breast brachytherapy1, indicating an advantage with GammaPod in further reducing the amount of radiation reaching critical organs and surrounding normal breast tissue.
Deep-Tissue Thermal Therapy
Enhanced Cancer-Eradicating Radiation
Deep-tissue thermal therapy can be especially useful in difficult-to-reach cancers in the abdominal and pelvic regions, including cancer of the bladder, rectum, cervix, ovaries, pancreas, and soft tissues. Studies have found that adding thermal therapy to standard treatments can significantly shrink tumors and can improve survival for some patients2. Thermal therapy – in the range of 104° up to 110° F. – sensitizes tumor cells to chemotherapy and radiation therapy. Additionally, heat has been shown to enhance the anti-tumor immune response.
Proton Therapy
The Only Proton Treatment Center in Maryland
Proton therapy is a highly advanced and precise form of radiation therapy that deposits all of its energy within the tumor and allows for less irradiation of surrounding normal tissue. Pencil-beam scanning proton therapy at the Maryland Proton Treatment Center allows University of Maryland radiation oncologists to deliver high doses of radiation that stop at the treatment site, protecting healthy tissue.
One of the many clinical benefits of proton therapy over conventional radiation treatments is a 26-39% decrease in secondary cancer risk3.
Combining Hyperthermia and Proton Therapy Could Mimic Carbon Ion Therapy Results
Carbon ion therapy delivers high amounts of energy that strikes tumors with a clustering effect, which can overwhelm the tumor's ability to persist or develop, especially damaging cancer cells at the DNA level.
A radiobiological rationale has been proposed suggesting that hyperthermia combined with protons could have effects analogous to high linear energy transfer (LET) radiation such as carbon ion therapy4. UMGCC offers the only center in the United States with the ability to combine these therapies for a seamless patient experience.
If you have a patient who could potentially benefit from any of our high-precision, advanced-modalities, consider referring them to UMGCCC. We will keep you informed of your patients' progress until they can be transitioned back to your care.
To Refer a Patient to the Department of Radiation Oncology at UMGCCC, call 410-328-6080 or 800-373-4111.
Related Content
- Learn more about the Department of Radiation Oncology at UMGCCC
- Schedule Grand Rounds for Your Hospital With Dr. Nichols for GammaPod or Miller for Proton Therapy
- Press Release: First Stereotactic Radiation Therapy System Designed to Treat Early Stage Breast Cancer Receives FDA Clearance
- FDA Approves GammaPod Breast Cancer Treatment
- UMMC a Leader in Offering Thermal Therapy
1Ödén J, Toma-Dasu I, Yu CX, Feigenberg SJ, Regine WF, Mutaf YD. Dosimetric comparison between intra-cavity breast brachytherapy techniques for accelerated partial breast irradiation and a novel stereotactic radiotherapy device for breast cancer: GammaPod™. Phys Med Biol. 2013 Jun;58(13).
2Datta N, et al. Local hyperthermia combined with radiotherapy and-/or chemotherapy: Recent advances and promises for the future. Cancer Treatment Reviews 41 (2015) 742–753.
3Eaton BR, MacDonald SM, Yock TI, Tarbell NJ. Secondary malignancy risk following proton radiation therapy. Front Oncol. 2015;5:261.
4Datta N, et al. Could hyperthermia with proton therapy mimic carbon ion therapy? Exploring a thermo-radiobiological rationale. Int J Hyperthermia, 2014; 30(7): 524–530.
