The University of Maryland Medical Center (UMMC) Obstetric Anesthesia team knows the birth of your baby is a very special time. Anesthesia specialists work on the UMMC Obstetric Care Unit every day. If a patient has medical issues that affect options for pain control, the OB doctor or midwife may ask the team to meet you earlier in pregnancy.
Labor Pain
Each woman’s labor is unique. Labor pain also feels unique for each woman. For some, the pain is manageable. Other times, pain medicines are helpful.
- How strong your contractions are
- Your baby’s size
- Your baby’s position
- Your past experience with pain
- Your beliefs and fears about labor
Types of Pain Relief
How can pain be treated without medicine?
- Deep breathing
- Warm showers
- Heating pads
- Massage therapy
- Counter pressure
- Changing position (walking, standing, sitting, rocking)
- Using a labor ball
Sometimes labor pain is too strong. Medicines to provide pain relief are often given by injection into an IV.
IV medicines are used in early labor to:
- Decrease the level of pain
- Make contractions more bearable
- Make the patient feel sleepy
Coming soon!
- Breathing nitrous oxide can help decrease labor pain
- Nitrous oxide and oxygen are administered through a facial mask
- Patients breath the laughing gas during contractions and breaths of normal air between contractions
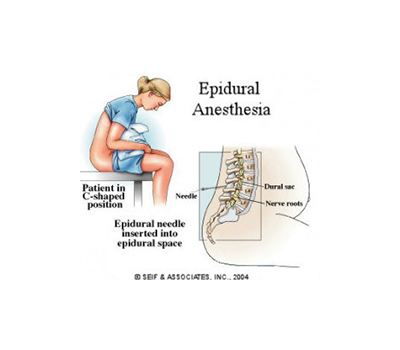
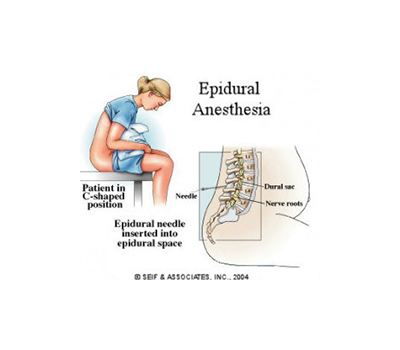
An epidural procedure is the practice of injecting medicine into the back of the patient to numb the lower part of the body. Medicines injected into the epidural space do not make the patient sleepy. Anesthesia experts administer these special medicines.
What is it like to have an epidural?
- Less intense labor pains
- Legs feel weak/heavy
- Pain relief without feeling sleepy
- Still feeling tightness and pressure with contractions
When can I get my epidural?
- Usually done during active labor
- Speak with the OB doctor, a midwife and an anesthesia doctor about timing
- If the child is crowning, it may be too late for an epidural
How are epidurals done?
- Support person goes to the waiting room
- Sitting on the edge of the bed the patient will arch their back into a C shape (see picture)
- Anesthesia specialists will numb the patients epidural space
- The patient will feel pressure in their back while the specialist locates the epidural space
- The anesthesia specialist will put in a thin plastic tubing (epidural catheter) into the epidural space
- Once the tubing is in place the needle is removed
- The anesthesia specialist will connect the epidural tubing to a medication pump
- Epidurals can take 15 to 20 minutes
- Epidural medicines take between 5 and 10 minutes to take effect
What does the nurse check after the patient receives an epidural?
- Numbness
- Pain levels
- Blood pressure and heart rate
- Ability to urinate
What are some epidural side effects?
- Feeling itchy
- Shivering
- Hard to pee on your own
- Low blood pressure
- Uneven pain relief
- Back pain
- Headache
- Bleeding or infection at injection site
- Nerve damage (extremely rare)
The healthcare team is prepared to treat any and all side effects.
Spinal Anesthesia is used for cesarean section (C-section) and is very similar to an epidural procedure.
- The spinal needle goes past the epidural space and into the spinal fluid
- Spinal medicine makes the lower body numb and weak
- Spinal anesthesia can make the patient numb enough to have surgery while conscious without pain
A cesarean section (C-section) is when a baby is delivered with surgery instead of labor. When a spinal or epidural cannot be done, the back-up option is general anesthesia (“going to sleep”).
This is when the Obstetric Anesthesiology team uses medicine to put the patient under until the C-section has been completed.