Anterior Cervical Fusion
A Patient's Guide to Anterior Cervical Fusion
Introduction
Most neck pain is due to degenerative changes that occur in the intervertebral discs of the cervical spine and the joints between each vertebra. The vast majority of patients who have neck pain will not require any type of operation. However, if the non-operative treatments fail to control your pain, your surgeon may suggest an anterior cervical fusion to try to reduce your neck pain.
The purpose of this information is to help you understand:
- The anatomy of the cervical spine
- The rationale for performing an anterior cervical fusion
- What you can expect from this procedure, including possible complications
Anatomy
In order to understand your symptoms and treatment options, you should start with some understanding of the general anatomy of your neck. This includes becoming familiar with the various parts that make up the neck and how these parts work together.
Please review the document, entitled:
Rationale
Surgery is not necessary in every case. No one type of surgery works for every neck pain problem. Numerous surgical procedures have been designed to treat each type of neck pain. An anterior cervical fusion is done for two reasons:
- To remove pressure from the nerve roots caused by bone spurs or herniated disc material
- To stop the motion between two vertebrae - a spinal segment
The Operation
Discectomy
One of the most common surgical procedures for problems in the cervical spine is an anterior cervical discectomy. The term "discectomy" means "remove the disc". A discectomy relieves the pressure on a nerve root by removing the herniated disc causing the pressure on the nerve root.
In the cervical spine, the disc is usually removed from the front. An incision is made in the front of your neck right beside your trachea (windpipe). The muscles are moved to the side. The arteries and nerves in the neck are protected as well.
Once the spine is reached from the front, each disc and vertebra are identified using an X-ray to make sure that the right disc is being removed. Once this is determined, the disc is removed all the way back to the spinal cord. Any bone spurs that are found sticking off the back of the vertebra are removed as well. Great care is taken to not damage the spinal cord and nerve roots.
In the cervical spine, a discectomy is usually combined with a spine fusion where the two vertebrae on either side of the disc that has been removed, are allowed to heal together, or fuse. The cervical fusion is described in detail below.
Anterior Cervical Fusion
Once the disc has been removed between the vertebrae, a cervical fusion is performed. This procedure allows the surgeon to fill the space left by removing the disc with a block of bone taken from the pelvis. Placing a bone graft between two or more vertebrae causes the vertebrae to grow together, or fuse.
The bone graft is usually taken from the pelvis at the time of surgery, but some surgeons prefer to use bone graft obtained from a bone bank. Bone graft from a bone bank is taken from organ donors and stored under sterile conditions until needed for operations such as spinal fusion. The bone goes through a rigorous testing procedure, similar to a blood transfusion. This is in order to reduce the risk of passing on diseases, such as AIDS or hepatitis, to the recipient.
For more information to help you understand bone graft please refer to the separate document, entitled:
There are two basic types of spinal fusion:
Anterior Interbody Fusion
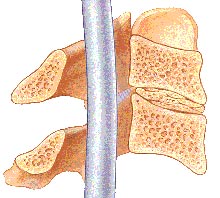
This type of fusion is much more common in the neck. This type of fusion is described above. In the interbody fusion, a bone graft is placed between two vertebrae and replaces the removed disc. During the healing process, the vertebrae grow together, creating a solid piece of bone out of the two vertebrae.
Posterior Fusion
You may hear the term posterior fusion as well. In the posterior fusion, the bone graft is placed on the back side of the vertebrae. During the healing process, the vertebrae grow together, creating a solid piece of bone out of the two vertebrae. This type of fusion is only rarely used in the cervical spine, generally only for fractures of the spine. If surgery is necessary, the anterior interbody cervical fusion is used to treat most problems in the neck caused by degenerative disc disease. These include unrelieved neck pain and pressure on the nerve roots caused by bone spurs or a herniated disc.
The goal of spinal fusion is to stop the motion caused by segmental instability. This reduces the mechanical neck pain caused from excess motion in the spinal segment. The anterior cervical fusion may also be done in a way that spreads the vertebrae apart a bit, trying to restore the space between them. Increasing the distance between the vertebrae also makes the foramen larger in the back part of the spinal column. This may reduce the pinching and irritation of the nerve roots by bone spurs around the foramen.
Instrumented Cervical Fusion
When doing a cervical fusion, the bone graft may simply be wedged in between the vertebra. It is held there simply because it is wedged in tight. In recent years, there has been an increase in the use of metal plates, screws, and rods to try to increase the success of helping the spine to fuse. Many different types of metal implants are used; all try to hold the vertebrae in position while the fusion heals. Bone heals best when it is held still, without motion between the pieces trying to heal together. The healing of a fusion is no different than healing a fractured bone, such as a broken arm. However, the neck is a difficult part of the body to hold still.
In the past, casts and braces were used in an attempt to reduce the motion in the neck and to increase the success rates of a spinal fusion. In most cases, these braces and casts were simply too cumbersome to wear for three months, and did a poor job of actually holding the neck still enough to allow the fusion to heal.
In the cervical spine, the most common form of internal fixation is using a metal plate and screws. The plate sits on the front of the vertebrae and the screws go backwards into the vertebral body to help hold the plate in place and to help keep the bone graft from slipping out of place.
By using metal plates and screws, the vertebra can be held rigidly in place while the fusion heals. Braces and casts are not needed.
Rehabilitation
For a more complete discussion of the rehabilitation programs for neck problems review the document, entitled:
Complications
With any surgery, there is a risk of complications. When surgery is done near the spine and spinal cord these complications (if they occur) can be very serious. Complications could involve subsequent pain and impairment and the need for additional surgery. You should discuss the complications associated with surgery with your doctor before surgery. The list of complications provided here is not intended to be a complete list of complications and is not a substitute for discussing the risks of surgery with your doctor. Only your doctor can evaluate your condition and inform you of the risks of any medical treatment he or she may recommend.
To understand more about the potential complications of spinal surgery, please review the document entitled:
Copyright © 2003 DePuy Acromed.
