Told You Have Prediabetes?

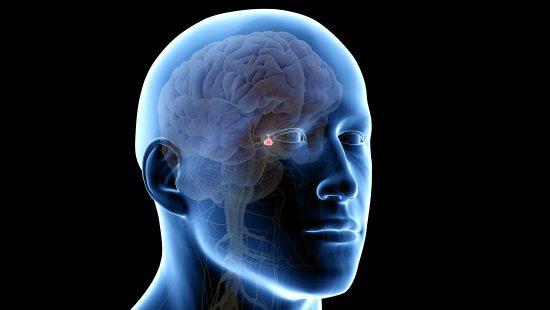
Sometimes called the master gland, the pituitary gland is about the size of a pea and located in the center of the brain behind the nose and eyes.
Because the pituitary gland regulates the hormones production, pituitary disease disrupts hormonal function, triggering a wide range of symptoms and conditions.
The far-reaching effects of pituitary disease mean that it can take a diverse team of specialists to treat it.
The University of Maryland Medical Center Midtown Campus's pituitary specialists are part of a multi-disciplinary center that diagnoses, evaluates and treats pituitary tumors and other disorders of the pituitary gland and the hypothalamus, the part of the brain that links the nervous system to the endocrine system.
Our multi-specialty team of specialists from neurosurgery, neurology, radiology and radiation oncology work together to offer you a comprehensive, personalized treatment plan.
Because the hormones that the pituitary gland controls affect everything from growth to sexual function, a pituitary malfunction can cause an array of conditions. Some of the most common ones we see include:
Depending on its size and location, a pituitary tumor can affect nearly any of the pituitary's functions, causing:
Diagnosis of a pituitary tumor involves blood tests, imaging, such as MRI and CT, and visual field testing.
Treatment ranges from monitoring to medications, surgery or in rare cases, radiation therapy.
When the pituitary gland produces too much growth hormone in adulthood it causes acromegaly. Its symptoms include:
Diagnosis of acromegaly involves blood tests and imaging, such as MRI and CT.
Treatment may include medications, surgery and/or radiation therapy.
If your pituitary gland decreases its production of growth hormone in adulthood, symptoms could include:
Diagnosis is made using an insulin tolerance test (ITT).
Treatment involves replacing the growth hormones with injection. Every four to eight weeks, the patient will return to the doctor for monitoring and a blood test to help the doctor decided if more hormone is needed or less.
Although similar in name to the more typical diabetes mellitus, diabetes Insipidus is a different disease. It is an imbalance of fluids in the body. Its symptoms are:
Diagnosis is made through medical and family history, physical exam, urine and blood tests, magnetic resonance imaging (MRI) and fluid deprivation test.
Treatment is usually medications.
When there is too much of the hormone cortisol — whether because of overproduction by the body or medications — Cushing disease can occur. The condition can in turn cause result in high blood pressure, bone loss and sometimes type 2 diabetes.
Its symptoms include:
Weight gain with fatty tissue around the midsection,, in the face and between the shoulders
Diagnosis is made through medical and family history, physical exam, urine and blood tests and magnetic resonance imaging (MRI).
