Neurosurgical and CNS Treatment Innovations Developed at the University of Maryland Department of Neurosurgery
For over 75 years, the University of Maryland Department of Neurosurgery has been at the forefront of advancing the field of neurosciences. Here are a few prominent innovations in neurosurgery and treatment of CNS conditions that have emerged through the decades because of the research and ingenuity of our physicians, scientists and inventors.
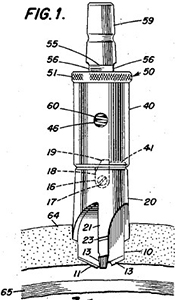
Automatic Drill for Craniotomy1
Though neurosurgeon George W. Smith, MD's initial patent filed in 1950 was called "Surgical Bone Perforator with Safety Stop" and later changed to "Automatic Drill", his invention became better known as the "Smith Drill" (Fig. 1). Prior to this innovation, craniotomies were created with instruments resembling carpentry tools, resulting in turning the bone into fine powder. With Dr. Smith's "osseous tissue drilling unit"2 , developed and tested while he was an instructor at the University of Maryland School of Medicine, extracted bone fragments could be preserved and replaced at incision closure to better facilitate patient healing. In addition, Smith designed his lightweight drill to automatically adjust its operation depending on the density of the tissue it was penetrating, and the drill was programmed to stop as soon as its base completely pierced the inner table of the cranium. It is not an overstatement to say that this device revolutionized neurosurgery.
Discovery of the SUR1/TRPM4 Ion Channel and Development of the SUR1/TRPM4 Inhibitor BIIB093 (Intravenous Glibenclamide) as a Promising Treatment for Cerebral Edema
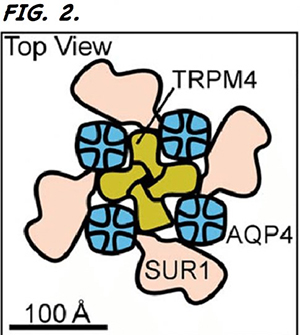
Through his basic research into the molecular mechanisms that cause secondary injury from CNS-related trauma, J Marc Simard, MD, PhD, Dr. Bizhan Aarabi Professor in Trauma at the University of Maryland School of Medicine, discovered the SUR1/TRPM4 channel and its role in causing CNS edema3. Currently, there is no reliable option for treating large hemispheric infarction (LHI), a severe form of ischemic stroke that comprises 14% of all strokes and has at least a 40% mortality rate. More than half of these LHI deaths are attributable to cerebral edema caused by the opening of the SUR1/TRPM4 channels. However, Dr. Simard's research contributed towards a proprietary formulation of glibenclamide – a common antidiabetic drug – that can be administered intravenously to inhibit the SUR1/TRPM4 channel (Fig. 2). After a successful phase 2 proof-of-concept trial in which subjects receiving IV glibenclamide experienced a 53% reduction in mortality, the FDA fast-tracked the agent. The formulation has been licensed to Biogen, which is now conducting the international, phase 3 CHARM clinical trial in 20 countries.
First Clinical Trials Exploring Focused Ultrasound to Disrupt the Blood Brain Barrier
Graeme F. Woodworth, MD, FAANS, FACS, Interim Chair and Professor of Neurosurgery at the University of Maryland School of Medicine, is leading the first clinical trials in the U.S. in which the blood brain barrier is disrupted to enhance brain tumor treatment. As 98% of FDA-approved drugs are unable to enter the brain because of this barrier, Dr. Woodworth is overcoming this obstacle through the use of microbubbles caused by focused ultrasound to create temporary openings via which agents can be delivered directly to tumor cells. Read more here about achieving blood-brain barrier disruption4 through focused ultrasound, a technology the UM Department of Neurosurgery also uses to treat essential tremor and Parkinson's disease.
To read about other neuroscience developments recently pioneered at the University of Maryland Medical Center, visit Physician Briefs.
1Smith GW. An automatic drill for craniotomy. J Neurosurg. 1950 May;7(3):285-6. PMID: 15415789.
2Smith GW, inventor. Automatic drill. US patent 2,842,131A. July 8, 1958.
3Chen M, Dong Y, Simard JM. Functional coupling between sulfonylurea receptor type 1 and a nonselective cation channel in reactive astrocytes from adult rat brain. J Neurosci. 2003 Sept;23(24)8568-77. PMID: 13679426.
4Harder BG, Blomquist MR, Wang J, Kim AJ, Woodworth GF, Winkles JA, Loftus JC, Tran NL. Developments in blood-brain barrier penetrance and drug repurposing for improved treatment of glioblastoma. Front Oncol. 2018 Oct;8:462. PMID: 30406029.
