eFocus – May 2023
Welcome to eFocus. Our goal is to provide you with timely, informative and useful short summaries and links about UM UCH related news, issues, or events. Feel free to contact us if you have news to share, story ideas or any other feedback. As always, your comments are welcome.
eFocus, May 2023 topics include:
WELCOME
Welcome to the May edition of eFocus. Warmer weather is coming, school graduation ceremonies are in preparation mode, and we are winding down the last two months of the fiscal year. We have much to celebrate! The reduction in Hospital Acquired Infections (HAI) remains one of the high points and we are on a record pace with regards to safety and quality. Our composite number is at 10 with 2 months to go. And, despite the challenges we have seen with staffing, the work by all of the teams to keep our patients safe has been exemplary.
During the month of April we did see a reduction in boarders at both Emergency Departments which did provide some respite; however, we continue to prepare both for the future winter months as well as the impending transition of Harford Memorial Hospital to the Aberdeen Medical Campus. That work is beginning in earnest as we know FY 24 will be a year of transformation of healthcare in Harford County.
Lastly, I recently had the pleasure and honor to volunteer for United Way's Project Connect at the Edgewood Epicenter with a great group of people from Upper Chesapeake Health, led by Christina Pedini. Take a look at some pics below. Thank you to all of the volunteers and dedicated staff that made this a complete success. Enjoy this month’s eFocus, and thank you for all that you do for our patients and community. See you in June!
Fermin Barrueto, Jr., M.D., M.B.A.
Senior Vice President/CMO
Medical Staff Affairs
DISCOVERY
UCH Mortality Survey Update – Learning from Every Death
There has been excellent engagement from providers and nurses who have been completing the mortality survey. Preliminary analysis showed that the most prevalent contributing factors were related to delays in care and missed opportunities for Hospice or Palliative Care Services. Improvement work groups with focus on palliative care/goals of care discussion and sepsis mortality have already been established.
If you are not the primary provider or nurse at the time of death but you have pertinent information to share related to the death of the patient, you could utilize the QR code available on flyers posted throughout the units. Thank you for your participation on this initiative to improve patient care. - UCH Quality Management Team

Hyperbaric Medicine Comes to UM Upper Chesapeake Health
This summer, UM UCH will open a Hyperbaric Medicine Center on the Bel Air campus. Equipped with state-of-the-art chambers, the spacious new facility will be managed by physicians and other providers specially trained for this advanced medical technology, ensuring patient safety and comfort in a close to home setting. It will be located in Pavilion II next to our advanced care Wound Center, and will treat outpatient conditions in collaboration with referring specialists from wound, vascular and podiatry centers, oral surgeons, urologists, plastic surgeons and primary care. Hyperbaric oxygen therapy is also frequently used as part of a combined care program that may include antibiotics and surgery. For more information, please call 443-643-3500 or review this flyer.
Lung Cancer Health Risk Assessment
If you have patients who may be at an elevated risk for lung cancer, consider sharing access to this free health risk assessment with them. Based on individual results, we may recommend an appointment with our Pulmonary Care and Sleep Medicine practice or a low-dose CT lung cancer screening through the lung cancer program here at UM UCH.

Oncology Grand Rounds, Cannabis Use and Oncology Care
Save the date and spread the word for Oncology Grand Rounds on May 10, 7:30-8:30 a.m. in the Streett Conference Room. The topic is: Cannabis Use and Oncology Care.
Learning Objectives:
- Examine the legislative impact of medical cannabis on the State of Maryland
- Define sativa, indica and hemp
- Review the evidence for cannabinoids in selected medical conditions
- Discuss future directions of cannabis and its role in medicine
See flyer for details.
COMPASSION
Patient Experience Week Recap
April 23-29 was Patient Experience Week, an annual event to celebrate healthcare staff impacting patient experience every day. UM UCH chose a theme of "Connecting to your WHY" (or purpose). Activities for the week included a viewing of keynote address by Jason Wolfe, President and CEO of the Beryl Institute on the Human Connection, having team members respond to the Tell Us Your WHY cards, deploying the UMatter Cheer carts to units/departments, service recovery training, and a celebration of Patient Experience Excellence awards. The week ended with an informative webinar on Trauma Informed Care by Dr. Toni Boulware Stackhouse, founder and CEO of Life Matters Wellness and a member of UM UCH Patient and Family Advisory Committee.
HVI Quality of Care Recognition (from a patient letter)
From the very first day I entered Cardiac Rehab, when my heart rate remained too fast to allow me to begin exercising, (whether I wanted to or not), and Katie K. called my cardiologist on my behalf, who subsequently adjusted the dosage of one of my medicines, and Jim made a follow up call to get clarification on exactly how that medicine needed to be taken, I knew I was in good hands, and in a safe place. My trust had been earned by the team, and allowed me to have confidence in process through which they would guide me.
My specific needs were ascertained early, and continuously reevaluated as they changed. I was treated with kindness, and respect, tempered with firmness when necessary, which was occasionally the case. When Katie K. had a rare day off, or was needed by a newer patient, other team members, Jessica, Katie S., Holly and Megan, were there for me. I was never, nor did I ever feel neglected. I was carefully monitored during exercise, and learned ways to warm up and cool down that will help keep me able to exercise safely on my own. Incremental increases in exercise difficulty were mutually decided on by Katie K. and I, at the end of each session. I was taught how to set up and start the machines I was using and increasingly encouraged to do so as independently as possible.
Katie K. was a wealth of information when she covered the topics in the Cardiac Rehabilitation Resource Manual, and readily answered questions I had. I also received much useful information from other team members.
Most important, however, are the results which I can feel every day. My mind is clearer. I breathe easier, have greater energy, less of the minor aches I was attributing to getting older, can climb stairs without any difficulty, can walk at a brisker pace and for longer, and am considering renewing activities, particularly drawing and painting, that I used to enjoy greatly. I fell I have been empowered through information and focused exercise, to continue building strength through informed choices and activity.
I am leaving Cardiac Rehab, and the people who make it work, not only with profound gratitude, but with great admiration and respect for both them and the work that they do.
Project Connect
On April 27, 15 team members from Upper Chesapeake Health volunteered to support the United Way of Central Maryland during their annual event, Project Connect. United Way of Central Maryland provides a community resource fair for Harford County residents who are experiencing or are at-risk for homelessness. Resources include housing and utility assistance, expungement services, health and vision screenings, COVID vaccinations, employment and training resources, treatment and recovery support for substance use issues, and more.


EXCELLENCE
Excellence in the Family Birthplace
Shoulder Dystocia is a known potential complication to a vaginal delivery; one or both shoulders get stuck behind the pubic bone during delivery. This is an OB emergency and can occur when the baby is large, in the wrong position or the mother has a small pelvic opening. There are maneuvers which the provider and nurse can perform to release the shoulders and in most cases the event last 60 seconds or less. A potential complication of a shoulder dystocia is a fractured clavicle or brachial plexus injury of the baby.
Recently, a patient and her baby experienced a shoulder dystocia that lasted 4.5 minutes. An OB STAT was called and team did an amazing job. The OB providers and CNM along with nursing, were able to deliver a 9 lb. baby who had no more than some facial bruising and a “stunned” look when he was fully delivered.
The teamwork from all who responded was amazing and because of their quick response and working together we had a mother and baby who after a very rough start, had an uncomplicated recovery and the rest of their stay was great. o show their appreciation to the team, 2 dozen fresh donuts were hand delivered the next morning.
Nominate a ‘Top Doctor’ for Baltimore Magazine
Baltimore magazine's 36th annual ‘Top Doctors’ survey is now underway for 2023. We hope that you’ll participate by nominating your physician peers across 100-plus specialties. The survey is available HERE. Last year, more than 250 individuals in 90 specialties and sub-specialties who provide care across University of Maryland Medical System hospitals were recognized as ‘Top Doctors’ in the November 2022 issue of Baltimore magazine. Twenty-six of them were on staff or had privileges at UM Upper Chesapeake Health. You can see the full 2022 list at umuch.org/topdocs. DEADLINE IS JUNE 2!
Safety and Quality Dashboard
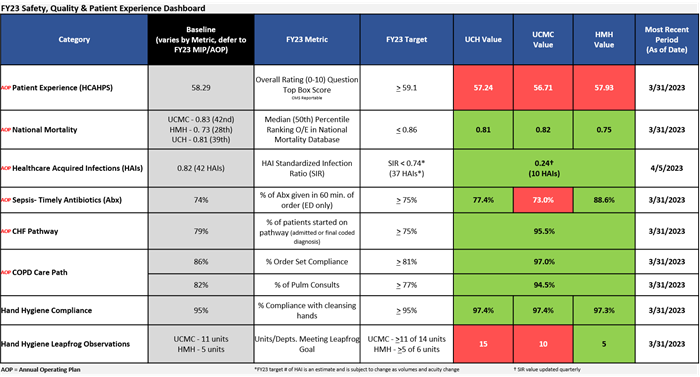
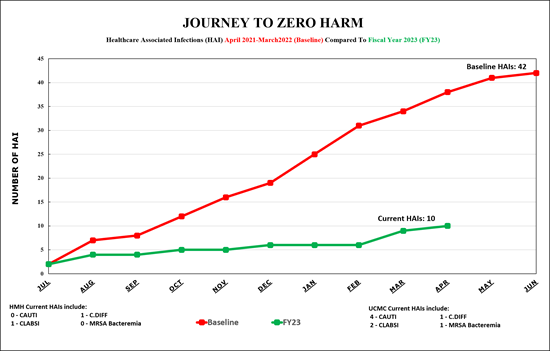
Healthcare Associated Infection (HAI) Prevention – Crushing it in FY 2023
As we near the end of the fiscal year, we are seeing great outcomes with our HAI prevention efforts. To date, we have 10 HAIs compared to 38 HAIs this same time in the baseline period, and we are on track to have our best performance year ever.
Now, we are in the “Final Countdown” to end the year, and we need to finish strong. Know your role in HAI prevention and stay focused. Be mindful of the following:
- Urinary catheters and central lines:
- Necessary – can an alternative be used
- Device order present with an appropriate indication
- Assess need daily
- d/c when no longer needed
- Culturing Stewardship
- Order for culture/test make clinical sense
- Infection Prevention Policies-follow them
- Hand hygiene
- Isolation precautions
- Stethoscopes—disinfect in between patient use
Thank you to all of those who have a role in this as it takes everyone doing their part to achieve this kind of success. Keep up the great work.
New TPN Committee
Contact the Total Parenteral Nutrition (TPN) committee when there is uncertainty about the direction of care for a TPN patient or a potential TPN patient. The TPN team is made up of an Intensivist, Pharmacist, Dietitian, Vascular Access Nurse and a Case Manager. Please utilize the TigerConnect Team “UCMC/HMH TPN Committee” to reach out to the stakeholders for guidance.
Medication Reconciliation Tips and Tricks - One Source of Truth
A crucial element for successful medication reconciliation is a single list to document a patient’s current medications. This list should be centrally located, accessible to those who participate in the care of the patient, and modifiable through the course of admission, thus becoming the “one source of truth.” Within EPIC, the Prior to Admission (PTA) Medications list serves as this source of truth.
A team approach is required for medication reconciliation, and this begins at patient presentation. While Medication History Technicians review and update the PTA medication list for 60% of admissions at UCMC on average, this leaves more than one-third of patients at UCMC and nearly all patients at HMH dependent on other care providers to initiate a thorough review of their medications. Keep this in mind when caring for a patient, and do not assume that someone else will take on this responsibility.
When reviewing the PTA medication list, be sure that all current medications, including supplements and OTC medications, are listed. Confirm the drug, dose, and frequency are correct and that when each medication was last taken is updated. The effort spent to have this information correct early on will go a long way in reducing the risk of medication errors.

New General Surgeon
Elizabeth Lowe, MD has joined Upper Chesapeake Surgical Associates. Dr. Lowe is a board certified general surgeon who has been in practice for over 20 years. She completed medical school at Tulane University School of Medicine and a surgical residency at East Tennessee State University / James H. Quillen College of Medicine.
Having had a rich presence in Cecil County, Dr. Lowe is beloved by generations of patients there. More recently she has been operating at University of Maryland Upper Chesapeake Health hospitals where she has developed an equally favorable reputation. Her office is now located in the Perryville Station complex on Pulaski Highway. Dr. Lowe has extensive experience with all general surgery procedures and formerly served as the Medical Director of the Union Hospital Breast Center. She has strong family values and is proud of the accomplishments of her two children. In addition, she enjoys boating on the waters of the upper Chesapeake Bay in her spare time.
Health Benefits of Walking Outside
Marie Kanagie-McAleese, MD, was quoted in the latest online edition of Reader's Digest / The Healthy in "7 Health Benefits of Taking Your Walk Outside." A board-certified pediatric hospitalist, Dr. Kanagie-McAleese also runs the county chapters of the Walk With a Doc program.
INTEGRITY
Pearls of Wisdom from Quality Management
As we all work toward better outcomes for our patients and in the spirit of process improvement, we would like to draw your attention to the below information which are findings gathered from case reviews.
- Changes in the plan of care should be communicated with the patient, caregiver and involved clinicians as well as documented in the medical record to ensure the continuity of care.
- Best practice for discharging patients includes prompt completion of the discharge work flow in order to ensure a safe hospital departure and a successful recovery. Essential items for discharge include the discharge order, medication reconciliation, diet and activity order.
- Indicate if a diagnosis was present on admission (POA), if documented after the H&P. Conditions are POA if identified in the Emergency Department, while in observation status and while having outpatient surgery. The clock starts when the admit to inpatient status order is written.
- Document ruled out for any differential diagnosis not confirmed, the Discharge Summary is the perfect place.
- It's very important to capture SIRS diagnosis on admission. It reveals your patient is at risk for many potential complications.
