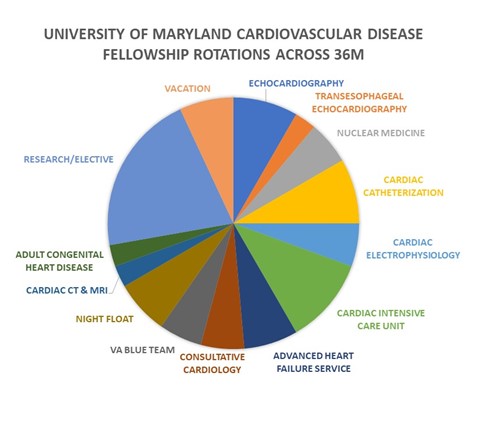
Rotations - Cardiovascular Disease Fellowship
Advanced Heart Failure Service (AHFS)
The AHFS rotation is an inpatient rotation focused on the care of telemetry patients with complex cardiac disease including, cardiomyopathies, pulmonary hypertension, complex arrhythmias, patients with advanced therapies such as left ventricular assist devices (LVADs), patients on intravenous inotrope or vasodilator therapies, and adult congenital heart disease patients. The Team is comprised of a Fellow and an APP is led by a Faculty in Advanced Heart Failure and Transplant Medicine. Fellows participate in the care of complex cardiac patients requiring advanced therapies like left ventricular assist devices (LVADs), evaluation for cardiac transplant and on intravenous inotropes or vasodilators for pulmonary hypertension.
Fellows engage in multi-disciplinary collaboration to provide optimal care for AHFS patients, interacting with other cardiac sub-specialties, pediatric cardiology, vascular surgery and CT surgery, as well as LVAD engineers.
This rotation comprises 8 weeks, divided over the course of first and second Years of Fellowship.
Cardiac CT | MRI
The Cardiac CT and MRI experience takes advantage of our imaging facilities at the affiliated Baltimore-VA Medical center as well as the downtown campus, with images from both sites reviewed by Attending Radiologists at the UMMC campus. Fellows integrate with CT Radiology fellows to review studies and complement the experience by providing clinical context for these studies. Some fellows choose to supplement this experience with through an external course to gain Level II training in Cardiac CT.
Consultative Cardiology
First year fellows spend two months rotating on the consultative cardiology service. A dedicated Nurse Practitioner and Fellow lead the service, with Internal Medicine house staff from the UMMC, Mid-Town Maryland, and Kaiser Internal Medicine residencies rotating on the service, along with University of Maryland medical students. Under the direction of an attending physician consultations across UMMC, Maryland Shock Trauma Center as well as an outpatient Prisoner’s Clinic are staffed. A wide array of pathologies is seen including acute coronary syndromes, pulmonary hypertension, arrhythmias and connective tissue and malignancy-associated cardiac conditions along with routine pre-operative cardiac risk-stratification, atrial fibrillation, and guidance for goal-directed management are managed by the Consult Team.
The service also offers opportunities for engaging in teaching medical house staff and medical students.
Cardiac Catheterization
During the first year of cardiac catheterization rotation, fellows are introduced to the sub-specialty at the Baltimore Veterans Affairs Medical Center. Second and third year cardiac catheterization rotations are based at the University Cath Labs.
Fellows participate actively in obtaining arterial and venous access and perform cases under the direct supervision of an attending interventionalist. Procedural competence obtaining access, utilizing vascular closure devices, and performing and interpreting right and left heart catheterization is obtained, as well as:
- Exposure to procedures such as pericardiocentesis
- Evaluation of coronary lesions with fractional flow wire and Doppler ultrasound
- Placement of Impella left ventricular assist devices and intra-aortic balloon pumps
- Endomyocardial biopsies
- Percutaneous coronary intervention
Fellows can engage in structural heart interventions including ASD/PFO closure, aortic and mitral valvuloplasty, TAVR and Mitra-Clip procedures.
Rotation objectives also include understanding the indications and contraindications to procedures performed in the Cath Lab, interpretation of coronary angiography and ventriculography as well as hemodynamic studies including constriction-restriction studies, valve interrogations, pulmonary hypertension and vasodilator challenge studies and exercise hemodynamics.
Formal cardiac catheterization rotation didactics include a weekly cardiac catheterization core conference, as well as a weekly clinical conference based on film review and clinical decision-making.
Cardiac Electrophysiology
Fellows are introduced to EP during their first year of training and then again in either their second or third years. Through this early exposure, fellows are able to inform decisions regarding pursuing cardiac electrophysiology as a career path based upon first-person knowledge.
The rotation is composed of consultative electrophysiology, involvement in diagnostic intracardiac studies and VT and SVT ablations, insertion and testing of pacemakers and internal defibrillators, and cardioversion. Each Thursday morning of the rotation begins with a discussion amongst all of the staff of the complicated cases, as well as a didactic session.
Cardiac Intensive Care Unit
The Cardiac Intensive Care Unit is a comprehensive experience in the care of acutely ill cardiac patients deriving from our advanced heart failure, pulmonary hypertension, acute myocardial infarction and severe valvular disease population. Multi-disciplinary care is delivered via a dedicated ICU team of physicians, APPs, nursing, PT, respiratory therapists and led by a general cardiology Attending Physician as well as an Advanced Heart Failure and Transplant Attending Physician. Trainees include Cardiovascular Disease fellows, residents and emergency medicine interns. Fellows rotate in the CICU all three years of training with graded levels of expertise and autonomy and participate in procedures, family meetings, as well as active management throughout the ICU stay.
Echocardiography
Fellows rotate in echocardiography in their first year, learning basic skills of wall motion analysis and ventricular function, evaluation of regurgitant and stenotic valvular lesions, intra-cardiac shunts, gradients, and pericardial disease. A core competency gained during this rotation is also to gain experience performing echocardiography and obtaining images, which is primarily garnered through joining sonographers on their echocardiography scans.
First year fellows also participate in the performance and evaluation of pharmacologic and exercise stress echocardiography.
Fellows in the second and third years of training who choose to participate in echo learn the skills necessary for performance and interpretation of trans-esophageal echo (TEE). They are also exposed to real time 3-D echo, dyssynchrony studies, TEE guided structural interventions including mitral, tricuspid, and left atrial appendage interventions, advanced tissue Doppler evaluations and advanced concepts such as speckle tracking.
The all-digital echo lab boasts more than 10,000 trans-thoracic studies, 1,200 trans-esophageal studies, and 1,200 stress echo studies annually. Studies are available for review anywhere within the hospital. Fellows participate in a weekly echo conference that incorporates didactic lectures with case study review.
Night Float
The Night Float rotation is structured with two providers in house, typically a Night Float Fellow along with another Fellow taking on an extra paid shift, an Attending Physician taking a paid shift, or an APP. These two providers cover the CCU, the telemetry Advanced Heart Failure patients, new admissions and Stat Echos and in-hospital consults. The Attendings of service are available for any coverage questions, as well as the Interventional Cardiology and EP Attendings on call. The rotation is scheduled as one six-day block at a time with 12 hour shifts scheduled 7pm to 7am.
VA Blue Team
The Blue Team is the cardiovascular medicine inpatient team for patients admitted to the Baltimore Veterans Affairs Medical Center, which is directly attached to the University of Maryland Medical Center. The Blue Team is composed UMMC Residency house staff, a team pharmacist, a cardiovascular disease fellow, and is led by a CVM Faculty Attending. Patients on the service are both Telemetry and ICU level. Fellows rotate on Blue Team during their second year and engage in several responsibilities, many affording them graded autonomy and independence. Blue Team fellows serve as team leaders for the Blue Team and have supervisory, patient management and didactic responsibilities towards the team. They additionally provide cardiology consultative services, along with the Blue Team attending, read inpatient and outpatient Echos, and triage inpatient device interrogation.
Fellows participate in 8 weeks of Blue Team rotation as second year fellows.
Nuclear Cardiology
Nuclear Cardiology is under the auspices of Radiology and is directed by Dr. Vasken Dilsizian, a renowned cardiologist who is also boarded in Nuclear Medicine.
On this rotation, fellows actively participate in all aspects of Nuclear Cardiology, from performance of dynamic tests to interpretation of myocardial perfusion scans, gated acquisition and PET scanning. Two months are required for cardiovascular fellowship training; however, most fellows choose to pursue an additional two months of nuclear training in order to fulfill requirements for eligibility for nuclear licensure and independent practice of nuclear studies.
Congenital Heart Disease
During this one-month rotation, fellows engage in outpatient and inpatient experiences with patients with congenital heart disease. This experience is multi-disciplinary with interactions with the Division of Pediatric Cardiology, including pediatric cardiologists, pediatric cardiac imaging specialists and pediatric interventional cardiologists, electrophysiologist and CT surgeons.
Fellows may participate in all aspects of Pediatric Cardiology including interpretation and performance of echocardiography, catheterization, and outpatient evaluation. The hallmark didactic conference of this rotation is a weekly multi-disciplinary meeting to discuss complex congenital cases of the week.
Research and Electives
Fellows choose electives according to career plans and academic interests. These may include increased exposure to any of the 'traditional' aspects of cardiovascular disease, such as cardiac catheterization, electrophysiology, echocardiography, transesophageal echocardiography and nuclear cardiology.
In recent years, trainees have utilized elective time to obtain training and certification in vascular studies through a collaboration with the Division of Vascular Surgery. Fellows have also chosen to spend more time in the interpretation of cardiac MRI and cardiac CT during these elective blocks. Additional elective rotations have included Pulmonary Hypertension Clinic, Cardiac Surgery ICU and Perioperative TEE.
Fellows have utilized research blocks expand their scholarship interests, including basic science research in extended blocks, and clinical and translational research.
Longitudinal Clinic
Fellows participate in a longitudinal clinic throughout their training, with 40-45 ½ day clinic sessions weekly. Clinics are suspended during Night Float, CCU, and AHFS rotations. Uniquely at our program, fellows follow a longitudinal patient panel at the Baltimore VA Medical Center as well as the downtown medical center practice. Through an innovative design exemption from ACGME, fellows alternate their half-day clinic between both sites, benefitting from the diverse demographic and pathologies served at each site. As elective experiences, trainees have also rotated to satellite clinics at the University of Maryland Practice in Westminster, MD.
Vacation
First year fellows have three weeks of vacation, as well as five wellness days to take at their leisure. Second and third year fellows are allotted four weeks of vacation. In the event of unexpected urgencies or emergencies, upper year fellows are also allotted five days of sick leave. Vacation is limited to two weeks at a time for first and second year fellows; during the last two weeks of June and first two weeks of July.
