Collaborative Approach Distinguishes Diagnosis and Treatment of Pituitary Tumors
University of Maryland Rounds features clinical and research updates from the University of Maryland School of Medicine and the University of Maryland Medical Center.
Intended for physicians, Rounds contains contact information to learn more about the clinical and research advances featured in each issue. It is printed three times a year and distributed monthly via email.
 When it comes to tackling pituitary tumors — a common type of brain lesion — it's unusual to find the collaborative, multidisciplinary approach distinguishing the University of Maryland Medical Center (UMMC) and its program to optimize treatments aimed at tumors in the body's "master gland."
When it comes to tackling pituitary tumors — a common type of brain lesion — it's unusual to find the collaborative, multidisciplinary approach distinguishing the University of Maryland Medical Center (UMMC) and its program to optimize treatments aimed at tumors in the body's "master gland."
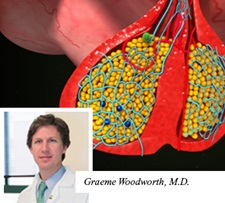
Between 300 and 400 cases of pituitary tumors are diagnosed and/or treated at the University of Maryland each year among a diverse group that includes young and old, both genders and every race, according to Graeme Woodworth, MD, an associate professor of neurosurgery at the University of Maryland School of Medicine.
Located at the base of the brain, the pea-sized pituitary gland is often referred to as the body's master gland because it regulates the balance of many hormones. "The vast majority of tumors we see are not cancerous, but they still greatly affect patients' overall health," explains endocrinologist Kashif Munir, MD, an assistant professor of medicine at the University of Maryland School of Medicine.
"We hold a multidisciplinary conference regularly to review cases together, laying out treatment options for each patient and discussing the options as a team -- which includes several neurosurgeons as well as specialists in endocrinology, oncology, ophthalmology, otolaryngology, radiology and radiation oncology -- so we can offer the best combined recommendation to each patient at each phase of care," says Dr. Woodworth, also director of neurosurgical oncology at the University of Maryland. "The broad spectrum of resources at UMMC is what differentiates our center."
Scans Vital to Diagnosis
Found in approximately 15% of individuals during autopsy studies — even if they never triggered symptoms — pituitary tumors are typically only diagnosed after a patient has noticed certain signs, which can range from mild to severe. Dr. Woodworth explains three common patterns precipitating diagnosis, including:
- Hormone imbalance: The pituitary releases an array of hormones affecting bodily functions such as growth, metabolism, egg and sperm production, breast milk production and the production of cortisol, a hormone with properties similar to steroids. Any of these processes can be disrupted by tumor pressure, causing a variety of symptoms.
- Headaches: During a medical workup for frequent headaches — which may be due to migraines or trauma such as an accident — a pituitary tumor may be discovered.
- New vision loss: The most alarming of the three patterns, vision loss is assessed with an eye exam and MRI scan of the brain. A pituitary tumor can prompt vision loss or double vision by pressing on optic nerves. "This can have a major impact on quality of life, because the patient can't drive and may not be able to work," Dr. Woodworth notes.
Regardless of presentation, diagnosing pituitary tumors commonly incorporates imaging scans such as CT or MRI. The latter is perhaps more effective, however, "because MRI is much better at visualizing soft tissue and brain structures," Dr. Woodworth says.
Surgery Tops Treatment Options
Among treatment options, surgery is tapped most often to accurately diagnose and treat pituitary tumors when indicated, Dr. Woodworth explains. He along with Drs. Francois Aldrich, Howard Eisenberg and Charles Sansur are the neurosurgeons consulted to handle these cases at UMMC. The most pressing indication for surgery is when a patient is suffering from a neurological problem such as vision loss from the mass. But when the tumor is clearly growing, surgery is indicated, as well as when a hormone imbalance is at play.
"For tumors that secrete hormones, we are often able to use the capsule on the outside of the tumor to obtain a complete resection, and potentially cure patients of their disease and help eliminate the need for repeat surgery," adds Dr. Sansur, an associate professor of neurosurgery. Typically, pituitary tumors are removed surgically through the nasal passage.
"The caveat is that prolactin-secreting tumors, which can stimulate breast milk production without pregnancy, may respond well to medical management with dopamine-related drugs," he says. Radiation therapy may also be used to treat pituitary tumors when surgery is deemed high-risk or in the case of recurrent tumors, Dr. Woodworth says.
In cases where radiation therapy is recommended, UMMC patients have access to proton therapy, a highly advanced and precise form of radiation, through the Maryland Proton Treatment Center (MPTC). MPTC offers the most advanced form of proton therapy in the world, called pencil bean scanning, which delivers powerful beams directly to tumors, protecting sensitive nearby tissues.
"There's also very exciting imaging research here to help predict which pituitary tumors are better candidates for certain surgical approaches and types of treatments. We using new MRI methods to look at the consistency of the tumor — whether it's firm or soft — and how that may impact surgical or radiation treatment," adds Dr. Woodworth.
"Yet some tumors may just need monitoring or medications to halt their growth," explains Dr. Munir. He adds, "What makes the University of Maryland stand out for pituitary tumor care is the number of experts working together to ensure patients get the best care possible."
For appointments, please call 410-328-6148.
Information about the Proton Center can be found by calling 410-369-5200.
