Postpartum Support
Making Women's Mental Health a Priority
A few days after giving birth to her first child, Christina Jones* sat in a rocking chair, shook her head furiously and cried to her husband that she couldn't "do this." Instantly overwhelmed by the changes that came along with having a baby, Jones felt as though she was physically separated from her body. Where was she? How could she escape from this life as a mom? Would she ever feel "normal" again?
In the next few months, instead of feeling sad and depressed, Jones felt anxious all the time. She would have near panic attacks when running errands with a fussy baby. It was a vicious cycle that stopped only for a short time and returned with the birth of her second child three years later.
But when Jones' second daughter was born, she was a little wiser and braver. "This time, soon after the baby was born, I didn't hesitate to call my doctor and cry to him on the phone," she says. "I knew I needed help, and I wasn't ashamed to ask for it."
*Not her real name
What is Postpartum Depression?
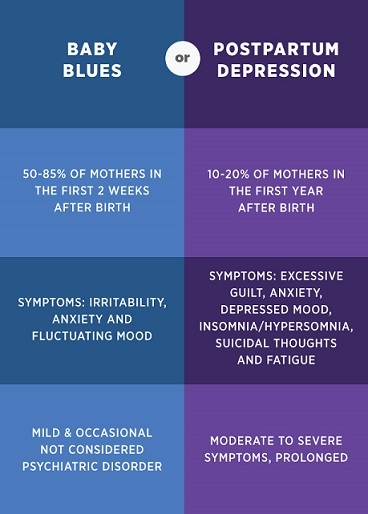
Postpartum depression (PPD) and postpartum anxiety (PPA) can be moderate to severe depression or anxiety that a woman experiences after giving birth. PPD and/or PPA can happen within the first few months after delivery or as long as a year later.
In the United States, about 70 to 80 percent of women will experience the "baby blues," feeling sad and somewhat overwhelmed with this new life adjustment. However, many women will develop the more severe conditions of PPD and PPA.
Some of the signs of PPD and/PPA may include:
- Feeling scared or panicky
- Not enjoying things you used to look forward to
- Feeling unusually sad, anxious or worried
- Having thoughts of harming yourself or your baby
Meeting the Needs of Women's Mental Health
Not every mother is able to reach out for help the way Christina did. Women who don't know how to get help or who may not fully understand what to call this condition may not know they can contact their OB-GYN. Some wives may have husbands and families that don't offer support, so they feel embarrassed to admit they need help? Plus, depression can occur during the pregnancy, something women may not be aware of.
Any woman who needs help with anxiety or depression at any time can call 1-800-NEXT-STEP.
