Care Management
Transform Health MD's Care Management Team — made up of nurse case managers, social workers and pharmacists — works with primary care providers and practice support staff to provide care planning and care coordination for attributed Medicare patients.
Services
The Care Management Team:
- Analyzes chronic disease status, risk-stratification tools, health care utilization and costs to proactively identify patients needing care management support
- Develops personalized, patient-centric care plans for high-risk, high-need patients benefiting from longitudinal relationship-based care
- Provides targeted short-term outreach and care management during risk periods
- Enhances health equity by identifying patients experiencing health disparities and helping them attain their highest level of health
General Approach
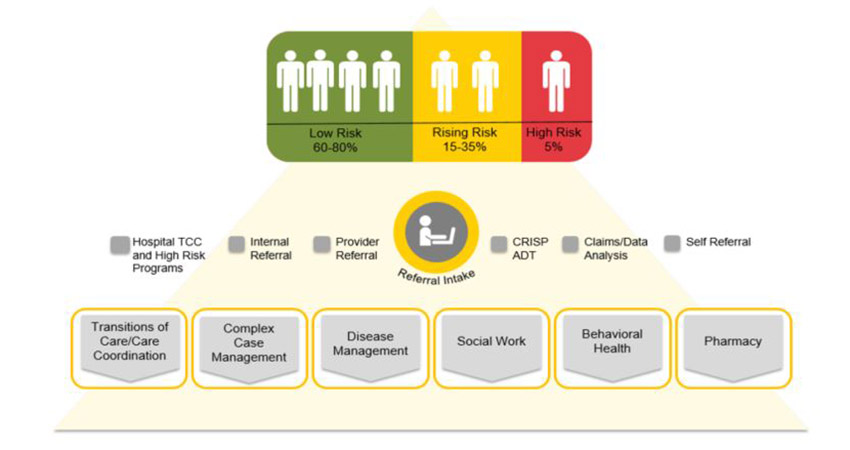
Two Step Stratification
Longitudinal Care Management
Longitudinal care management involves developing personalized care plans for high-risk, high-need patients aimed at providing regular, proactive outreach and longitudinal relationship-based care. Often, patients have conditions or situations whose outcomes can be modified through patient-provider-care manager collaboration and engagement.
Those who can benefit from longitudinal care management typically have:
- Complex treatment plans
- Multiple comorbidities
- High inpatient and emergency room utilization
- Mental illness or behavioral health needs
- Complex medication regimens
- Socioeconomic risk factors influencing overall health
The Care Management Team works with patients and families, primary care providers, hospitals, specialists and community agencies to help coordinate care and services.
Episodic Care Management
The Care Management Team provides targeted short-term care management to support patients through a period of risk. This includes:
- Brief disease management and health coaching
- Outreach and education for new diagnoses
- Medication reconciliation (a medication review with the patient/caregiver to establish an updated medication list) on transitions or for polypharmacy (use of multiple drugs at once to treat a single condition)
- Coordination and accurate information sharing during transitions of care (e.g., from hospital to home and post-acute care settings)
- Connection to community resources, transportation and specialty referral coordination